Request Appointment
Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.


Do you know we have 23 cushions like the spinal disc in our spine?
Six in the neck or the cervical region, twelve in the mid back or the thoracic region and five in the lower back or the lumbar region.
They support us by acting as a shock absorber of our body, transferring the weight, prevents the friction between two vertebrae during any movement, and allowing us to jump, bend, turn and twist.
These spinal disc or intervertebral disc as called scientifically is jelly like a cartilaginous structure present in between two spine bones or vertebrae. A disc is made up of a thick outer ring of fibrous cartilage called the anulus (derived from the Latin word “anus” meaning “ring”), which surrounds an inner gel-like center or more gelatinous core called the nucleus pulposus (meaning “pulpy interior”). The nucleus pulposus is wedged between cartilage endplates on both sides as its roof and floor.
They are located in our neck, mid back as well as lower back, adding one third to one quarter of the total height of the spine.
Since these intervertebral discs are an important structure, any problem in the disc can disrupt the normal function of the spine.
There are various types of disc problems that one can experience in the form of pain in the neck, the mid, the lower back, and pain radiating down the arms or leg like sciatica.
These disc problems can be pathological, chemical in nature such as infection, or mechanical in nature, which gets better with spine rehabilitation. Following are the types of disc conditions:-
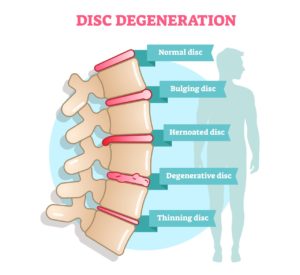
Bulging disc or slipped disc
Disc bulge or slipped disc are is a condition when the disc forms a budging appearance due to increased pressure on the disc. Disc budge is often mistaken as herniated disc as the symptoms overlap. Slip disc treatment varies based on the level and extend of pressure on the disc, out of which exercise for disc problems are most reliable.
Herniated disc or gel is out or pinched nerve
When the gel-like substance of the nucleus pulposus is pushed out of the encircling anulus fibrosus, it might exert pressure on a neighboring nerve, resulting in a spinal disc herniation. If it presses against the roots of the sciatic nerve, it might cause sciatica symptoms.
Symptoms may appear in different parts of your body depending on where your bulging disc is located. You may feel similar feelings in your lower back, legs, buttocks, and feet if your bulging disc is in the lumbar area. These symptoms may appear in your neck, arms, or hands if it is in your cervical area. You could even see them in your head in certain situations.
Degenerative disc
Around a quarter of the world population under the age of 40 have signs of spinal disc problems due to disc degeneration at one or more levels. On magnetic resonance imaging, an imaging investigation more than 60% of adults over the age of 65 show signs of disc degeneration at one or more levels.
The nucleus pulposus or the inner gel of the disc starts to dry as a result of ageing, reducing the disc’s capacity to absorb shock. This overall shrinkage of disc size contributes to the normal decline in height as people become older.
With ageing, the annulus fibrosus or the outer layer of the disc gets weaker and is more prone to ripping. Furthermore, the cartilage endplates begin to weaken, cracks, and the subchondral bone of the vertebrae begins to wean off. In nutshell, significant wear and tear take place in the disc due to aging.
Thinning of a disc, water content is less, may or may not have pain, stiffness
Thinning discs are usually attributed to nothing more difficult than the normal ageing process. Intervertebral discs lose hydration in their gel-filled cores over time, and the discs’ tough outer shells fracture and become brittle.
Pain, numbness, tingling, and weakness are common symptoms of thinning disc-related spinal injuries, which can result in significant mobility loss and a worse quality of life.
Discitis
Infection or inflammation of the spinal disc is called discitis or diskitis. Swelling in the affected disc exerts pressure on the surrounding structure leading to irritation and inflammation of soft tissues, joints, and vertebrae at the site. This condition usually presents with pain, swelling, stiffness at rest and fever.
When one or more of your discs are damaged, it can have a variety of negative consequences in your life, including the following symptoms:
The discomfort or soreness is felt around the damaged disc is the most common sign of a herniated disc. If a herniated disc pushes on the spinal cord, it can result in muscular weakness, numbness, or tingling, enhanced leg reflexes, bladder or bowel function abnormalities, or even paralysis if left untreated.
A detailed physical examination by a spine specialist and imaging investigation like MRI confirms the diagnosis, and then the treatment is planned accordingly.
Conservative treatment is the first line of treatment for disc problems.
Physical therapy, cold and heat therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), Skeletal muscle relaxants and epidural injections are all options for conservative management of a herniated disc as well as slip disc treatment.
Relative rest is recommended as first aid when you are allowed to be active but avoid physical exertion, and aggravating factors such as repetitive bending, lifting weights and prolonged sitting on the sofa, bed, or recliners.
If 6-8 weeks of non-surgical therapy fails to relieve herniated disc symptoms, microdiscectomy surgery is typically advised. The herniated portion of the disc is removed during this operation to alleviate pressure on the nerve root and allow it to recover. Post- operative care includes mild exercises which are prescribed by spine specialist physiotherapist in collaboration with your surgeon.
Having said that, most of spinal disc problems can be treated non-invasively based on short and long term relief.



Dosage: 10 repetitions on each side, twice a day.
Prevention like any other medical condition is better than cure. With active lifestyle, the use of ergonomic workstation and a fitness regimen focusing on spine health is proven to reduce the risk of spinal disc problems. A spine rehabilitation specialist designs such regimen.
Who are Spine specialists and when to seek their advice?
A spine rehabilitation specialist is a registered physiotherapist with extensive training and advance degree in spine rehabilitation. Since most spinal disc problems can be treated without medicines and surgeries, it recommended to visit a spine specialist for pain reduction, achieving complete recovering and recurrence management. Even if one is prescribed surgery, it is safe to seek a second opinion.
If you are able to relate to any of the spinal disc problems, book your appointment with a spine rehabilitation specialist near you at QI Spine Clinic.
Clinical inputs on this article is given by Dr Sara Ansari, PT, Spine Rehab Specialist.
Visit our nearest clinic for your first consultation