Request Appointment
Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.


The coronavirus disease 2019 (COVID-19) pandemic and the subsequent lockdown of 2020 had enforced social distancing and severe travel restrictions to control the spread of the virus. This led to a significant decrease in patients visiting healthcare centres and clinics and an increased adoption of telemedicine-based platforms to remotely deliver healthcare to the population to minimize the risk of virus transmission [1,2]. Similarly, the use of telemedicine-based platforms to diagnose and treat musculoskeletal conditions such as spine pain has also increased during the COVID-19 pandemic [3–5]. Negrini et al. [5], in an analysis of telerehabilitation provided to paediatric patients with spine disorders, reported that outpatient-type teletreatment was feasible with a high level of patient satisfaction. Similarly, Bhuva et al. [4], in a prospective cohort study of 172 patients with spine pain, reported that telemedicine provided effective and satisfactory physical rehabilitation care.
However, telerehabilitation for spine pain has its challenges and disadvantages when compared to in-person, outpatient-based evaluation and rehabilitation. These include the lack of direct person-to-person contact which makes it more difficult to build a strong patient-clinician relationship, a limited amount of clinical examination tests and diagnostic movements that can be performed, lack of equipment and devices that can be used as part of therapy, and a limited amount of therapeutic exercises that can be administered, all of which may impact the diagnostic process and treatment outcomes of spine rehabilitation [6–8]. Furthermore, online consultation and treatment from patients’ homes, especially in low-resource settings, may pose additional challenges of internet connectivity and cultural and lang barriers towards acceptance and delivery of health services through a telemedicine platform [9].
Despite increased advocacy and usage of telemedicine-based platforms to deliver rehabilitation treatment during the COVID-19 pandemic [1,10], the efficacy of telerehabilitation for spine pain in comparison to outpatient-based, in-person rehabilitation is unknown. Few recent studies have compared clinical outcomes in online versus in-clinic instruction of exercises in patients with low back pain (LBP) [11–14]. However, most of these studies were conducted in the pre-COVID-19 pandemic period and the online or telerehabilitation platform in them was used to instruct patients on the technique of performing home exercises rather than as a method to remotely and comprehensively diagnose and treat patients for spine pain [11–14]. Hence this study aimed to determine the effect of telerehabilitation on pain and disability in patients with spine pain treated during the COVID-19 pandemic and compare the results to in-clinic multimodal spine rehabilitation. We hypothesized that our telerehabilitation protocol would be effective in reducing pain and disability in patients with spine pain, similar to outpatient-based multimodal rehabilitation.
This propensity score-matched analysis was conducted using electronic records of 470 patients treated conservatively with telerehabilitation for spine pain by a team of spine physiotherapists during the 6-month lockdown phase of the COVID-19 pandemic from April 2020 to September 2020. As a control, electronic records of 4035 patients treated conservatively with outpatientbased rehabilitation for spine pain by the same team at a chain of spine rehabilitation clinics (QI Spine Clinic, India) during the 6 months just before the lockdown from October 2019 to March 2020 were used. The study protocol was approved by an institutional review board and ethics committee (Ethics committee project number: MMCRI/IEC/2021-22/008).
The study population for this retrospective study was individuals who approached us for evaluation and treatment of their acute or chronic spine pain during the 6-month period prior to the COVID19 lockdown from October 2019 to March 2020 in the in-clinic rehabilitation or control group or over a teleconsultation platform during the 6-month lockdown phase of the COVID-19 pandemic from April 2020 to September 2020 in the telerehabilitation group. For the telerehabilitation group, the inclusion criterion was all patients with mechanical spine pain who underwent rehabilitation treatment using a teletreatment platform whereas the inclusion criterion for the in-clinic rehabilitation or control group, was patients with mechanical spine pain who underwent in-clinic multimodal rehabilitation treatment. The exclusion criteria were similar for the 2 groups and were patients with “red flag” conditions (tumour, infection, trauma or fracture, cauda equina syndrome, progressive neurodeficit), inflammatory conditions (ankylosing spondylitis, rheumatoid arthritis), significant motor deficit with muscle strength grade <3, peripheral joint involvement, structural kyphotic or scoliotic deformities, peripheral neuropathy, lumbar canal stenosis (diagnosed clinically based on presence of neurogenic claudication and findings of central canal stenosis on magnetic resonance imaging), complex pain syndrome, previous spine surgery, incomplete clinical records, and patients who did physiotherapy for <6 sessions or >36 sessions.
To minimize the possibility that pain and disability had improved with time rather than with rehabilitation treatment, patients who underwent >36 treatment sessions were excluded. Furthermore, patients who could not complete their evaluation due to poor comprehension or logistical problems such as poor internet connectivity or inability to use the telemedicine platform were also excluded in the telerehabilitation group.
Mechanical spine pain was defined as spine pain arising intrinsically from the spine or surrounding soft tissues which worsened with specific spine movement and improved with rest whereas non-mechanical spine pain was spine pain due to an underlying inflammatory (e.g., rheumatoid arthritis or spondyloarthropathies) or red flag conditions [15]. Based on the inclusion and exclusion criteria, data from clinical records of patients who underwent treatment for their mechanical spine pain in the control and telerehabilitation groups were analysed for this study.
In the telerehabilitation group, the first consultation was conducted by a physiotherapist who evaluated and diagnosed all patients using a standardized protocol designed for teleconsultation. All physiotherapists in the telerehabilitation team were trained in the evaluation, diagnosis, and treatment of patients with spine pain before the start of this service to maintain standardisation. A day before the consultation, all patients were sent a Google form (Google LLC, USA) link containing a questionnaire to record demographic details, details of presenting complaints and symptoms, medical and surgical history, and questions to screen for red flag conditions. Clinical evaluation was performed using free teleconference apps such as Zoom (Zoom Video Communications Inc., USA) or WhatsApp (WhatsApp Inc., USA) using a standard clinical examination checklist (Figure 1).
To ensure that ethical best practices were followed during telerehabilitation, an informed consent for the use of communication applications for consultation and treatment was taken from all our patients. Professional patient-care giver confidentiality during all communications was ensured by using secure communication applications such as Zoom (Zoom Video Communications Inc., USA) or WhatsApp (WhatsApp Inc., USA) which were acceptable for delivering teletreatment during the COVID-19 pandemic lockdown [16], and none of the teleconsultation or treatment sessions were recorded by the physiotherpist. Patient data safety was ensured by storing all patient related data in a proprietary electronic medical record (EMR) system developed and used only by our chain of clinics, which prevented third-party ownership and access to our patient data. Furthermore, patient data access was given only to their caregivers involved in their telerehabilitation.
Clinical examination included identifying directional preference (DP) based on the Mechanical Diagnosis and Therapy (MDT)VR technique [17,18]. Similarly, for in-clinic consultation, all patients were evaluated and diagnosed by a trained senior spine physiotherapist using a standardized protocol similar to the one previously mentioned for teleconsultation.
In the telerehabilitation group, all patients were treated by senior physiotherapists experienced in spine rehabilitation and who underwent training in the spine telerehabilitation protocol. This novel spine telerehabilitation protocol (Figure 1) was a
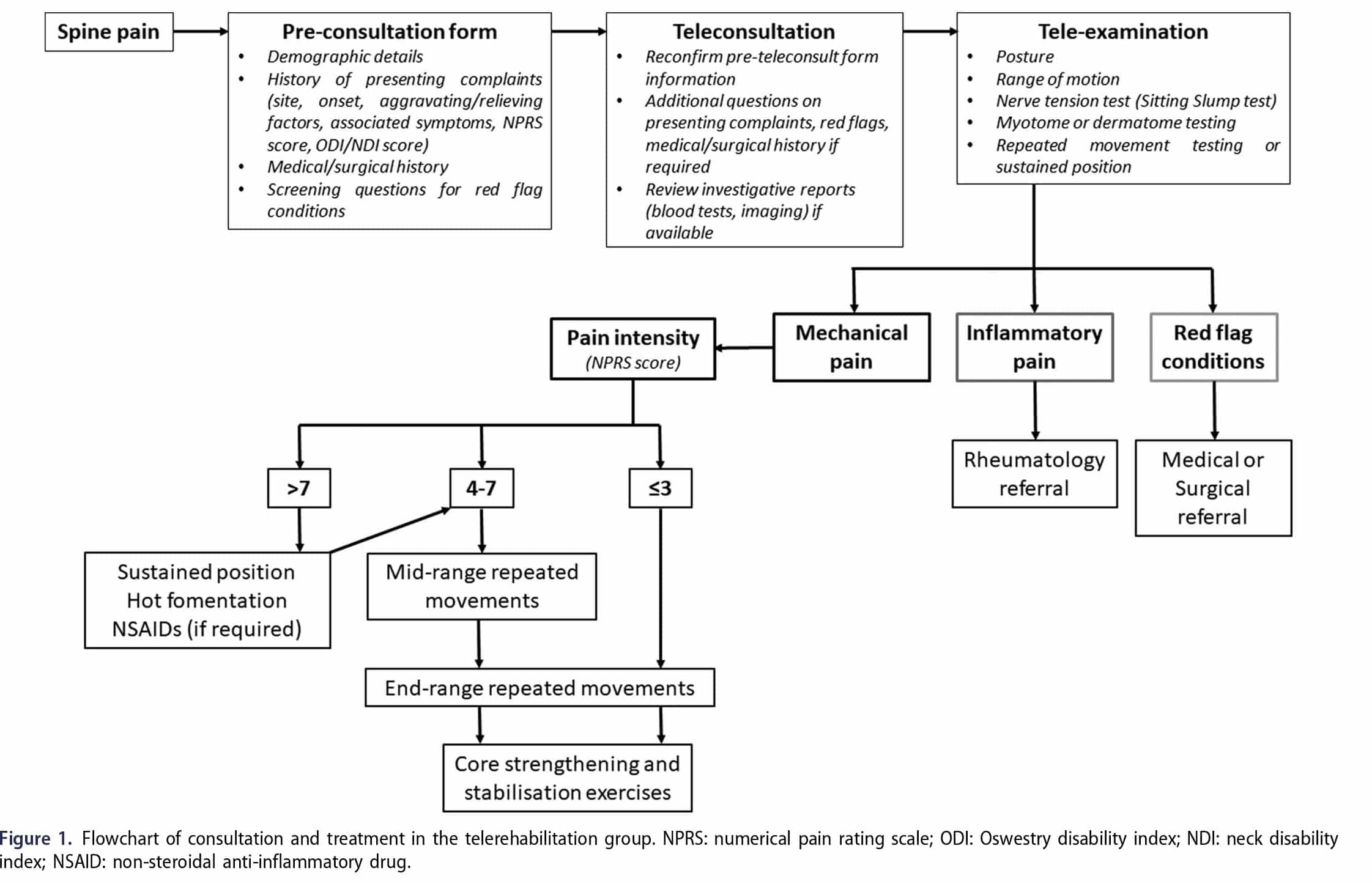
modification of our in-clinic spine rehabilitation protocol and was designed by senior members of the team to account for the restrictions and challenges which the teleconference apps posed during the evaluation and treatment process. The spine telerehabilitation protocol included – (1) patient education, (2) pain reduction using repeated movements or sustained positions based on DP identified using the MDT technique, and (3) core strengthening and stabilization exercises. All patients were educated about maintaining proper posture, avoiding pain aggravating movements, and taking regular breaks when required during daily activities at home or work.
Pain intensity was measured using the numerical pain rating scale (NPRS) ranging from “0” (no pain) to “10” (worst pain imaginable) [19]. Based on previously published reports, pain intensity was categorized as mild pain with NPRS score �3, moderate pain with NPRS score 4–7, and severe pain with NPRS score >7 [20,21]. In patients with severe pain (NPRS score >7), DPbased sustained postures were prescribed rather than repeated movements, and patients were advised to apply hot fomentation after the session to prevent aggravation of pain. All patients were advised to perform repeated movements 4–5 times a day if the pain was moderate (NPRS score <7), starting from mid-range movements and slowly progressing it to end-range repeated movements. As the pain reduced over time, core strengthening exercises (2 times a day) were added, and the intensity gradually increased from basic to intermediate to advanced level. Core strengthening exercises included basic exercises such as core activation, isometric activation of internal and external oblique muscle, core activation with bridging and clams and intermediate and advanced core exercises such as progression of bridging prone and side planks, abdominal and oblique crunches, opposite arm and leg raise in all fours position, and core with staright leg raise and abduction. Similarly, for patients with neck pain (NP), basic, intermediate, and advanced strengthening exrecises for the neck and upper back were administered. All patients were advised 2–3 supervised telerehabilitation sessions a week and a minimum of 6 total treatment sessions. During each session, the treating physiotherapist gave a real-time demonstration of new exercises being prescribed and all patients were provided with a digital document illustrating various exercises which the patient could access during their home exercises.
For the in-clinic treatment, all patients were treated using a multimodal rehabilitation protocol by physiotherapists experienced in spine rehabilitation and trained in using a standard treatment plan of care. The multimodal protocol included – (1) patient education, (2) pain reduction using frequency-specific microcurrents (FSM) [22,23], and repeated movements or sustained positions based on DP identified using the MDT technique, (3) device-based and manual strengthening and stabilization exercises, and (4) home exercise and self-care training. If the intensity of spine pain was severe (NPRS score >7), FSM therapy and low-intensity extension mobilization exercises were started during the first week of treatment for pain management. These patients were also started on repeated movements based on their DP performed under supervision by the treating physiotherapist and to be continued at home at least 4–5 times a day, till NPRS score reduced to <4. Once the pain reduced to mild (NPRS score � 3), device-based strengthening and stabilization exercises were initiated. All patients were advised to continue strengthening exercises at home at least 2 times a day. Adherence and technique of home exercises was verified by the treating physiotherapist during each session to make sure the patient was compliant with the home exercises prescribed during the previous session and any deviations found were corrected. All patients were administered a minimum of 2–3 supervised in-clinic treatment sessions per week and a minimum of 6 total treatment sessions.
Baseline variables including demographic covariates such as gender, age, location of pain, pain intensity measured using the numerical pain rating scale (NPRS) [19], and disability measured using the Oswestry disability index (ODI) score for LBP or Neck disability index (NDI) score for NP with or without upper back pain (UBP) [24,25], were collected from all patients at the time of the first consultation. Total treatment sessions and treatment duration were also collected for all patients. Participants’ pain intensity and disability scores were obtained post-intervention by their treating physiotherapist. To determine the change in outcome variables (NPRS and ODI/NDI scores) at the end of treatment when compared to baseline values, the minimal clinically important difference (MCID) between pre-and post-treatment NPRS and ODI/NDI scores were calculated. Based on the recommendations by Ostelo et al. [26], MCID thresholds were set at 2 points improvement for NPRS score and 10 points improvement for ODI/ NDI score from pre-treatment values. Based on recommendations by Asher et al. [27], for comparison between the 2 groups based on pre-treatment NPRS and ODI/NDI score subgroups, the MCID was set at �30% between the pre- and post-treatment scores.
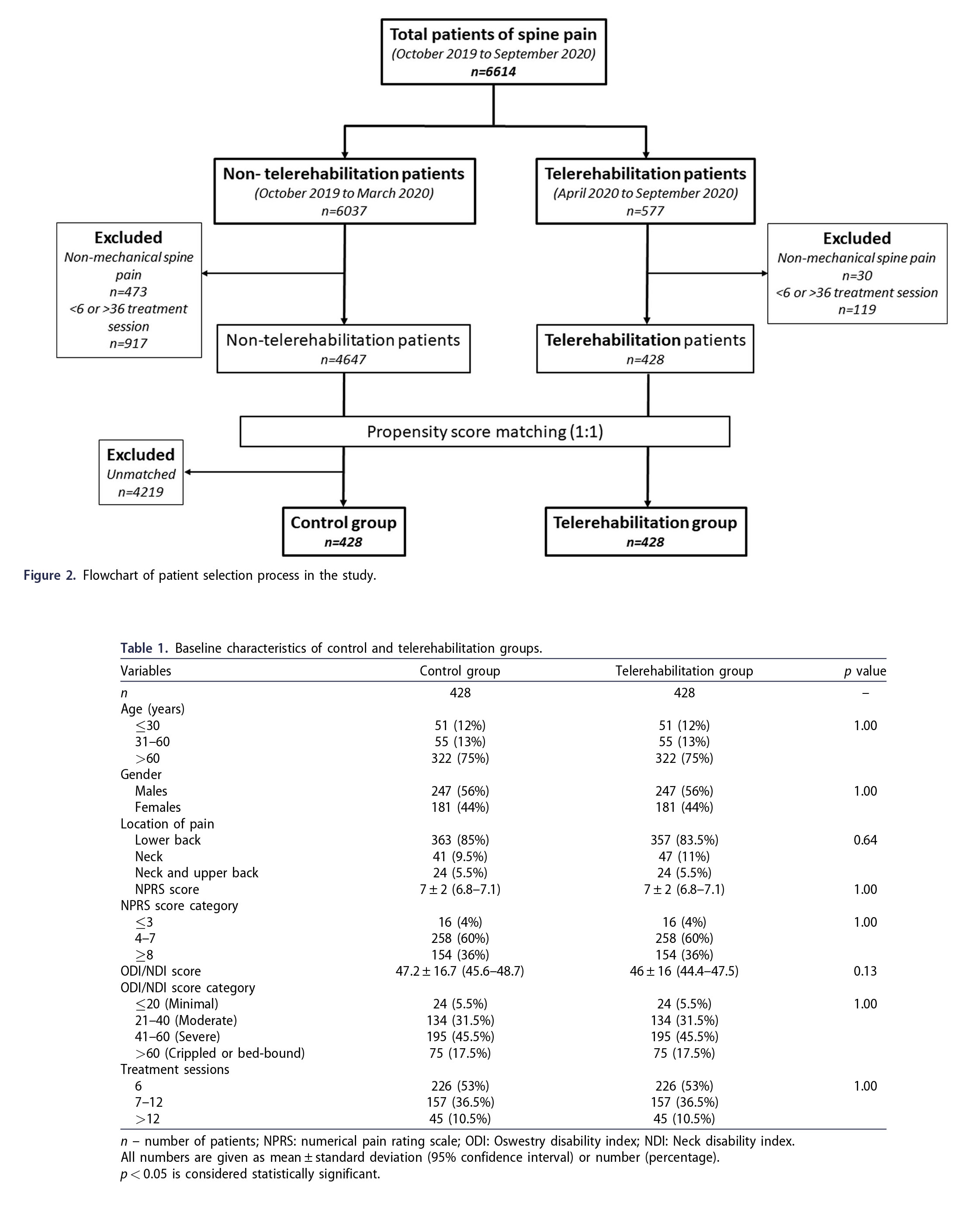
The propensity score matching method was used to select the control group from the patient population who underwent nontelerehabilitation treatment for spine pain. The propensity score was calculated according to gender, age, pre-treatment NPRS, ODI/NDI scores, and number of treatment sessions and then a 1:1 matching was performed. Age was classified into �30, 31–60, and >60 year groups, pre-treatment pain was classified into mild (NPRS score �3), moderate (NPRS score 4–7), and severe (NPRS score �8), pre-treatment disability was classified into minimal (ODI/NDI score �20), moderate (ODI/NDI score 21–40), severe (ODI/NDI score 41–60), and crippled/bed-bound (ODI/NDI score >60), and number of treatment sessions was classified into 6, 7–12, and >12 sessions.
Baseline demographic and pre-treatment variables such as age, gender, number of treatment sessions, NPRS, and ODI scores were compared between the 2 groups. Similarly, outcome variables such as post-treatment NPRS and ODI scores, percentage of patients who achieved MCID thresholds for NPRS and ODI scores, and the percentage of patients who achieved an MCID for NPRS and ODI scores based on pre-treatment NPRS and ODI/NDI subgroups were compared between the 2 groups. Pre- and posttreatment variables were also compared between the 2 groups based on specific pain locations (LBP, NP, and NP with UBP). Categorical data were compared using the Chi-square test and continuous data were compared using one-way analysis of variance (ANOVA). A p-value of <0.05 was considered significant. Statistical analysis was performed using the GraphPad QuickCalcs online statistical analysis tool (GraphPad Software, San Diego USA).
Based on the inclusion and exclusion criteria, 4647 patients in the control group and 428 patients in the telerehabilitation groups were available for matching (Figure 2). After propensity score matching, data from 428 patients each in the control and telerehabilitation groups were compared for this study (Figure 2). Comparison of baseline parameters between the 2 groups is summarized in Table 1. There was no significant difference in the distribution of patients among subgroups for age, gender, location of pain, NPRS score, ODI/NDI score, and number of treatment sessions when the two groups were compared (Table 1). The mean treatment sessions done in both groups were similar at 9 sessions and the mean treatment duration was 6.5 weeks in the control group and 7.5 weeks in the telerehabiltation group.
Post-treatment, the mean NPRS (mean difference 1, p < 0.0001) and ODI/NDI (mean difference 5.8, p < 0.0001) scores, were significantly lower in the telerehabilitation group when compared to the control group (Table 2). Similarly, the percentage of patients who achieved MCID of � 2 for NPRS (mean difference 6%, p ¼ 0.0007) and MCID of � 10 for ODI/NDI (mean difference 7.5%, p ¼ 0.005) scores were significantly higher in the telerahbilitation group when compared to the control group (Table 2).
Based on pre-treatment NPRS subgroups, a significantly higher percentage of patients with pre-treatment NPRS 4–7 (mean difference 7.5%, p ¼ 0.001) and NPRS �8 (mean difference 13%, p < 0.0001) achieved an MCID of 30% for NPRS score in the telerehabilitation group when compared to the control group (Table 2). Based on pre-treatment ODI/NDI subgroups, a significantly higher percentage of patients with pre-treatment minimal disability (mean difference 29%, p ¼ 0.03), severe disability (mean difference 12%, p ¼ 0.002), and crippled/bed-bound disability (mean difference 13%, p ¼ 0.04) achieved an MCID of 30% for ODI/NDI score in the telerehabilitation group when compared to the control group (Table 2).
The mean pre-treatment NPRS score were not significantly different when the two groups were compared based on LBP (p ¼ 1.00), NP (p ¼ 0.15), and NP and UBP (p ¼ 0.57) (Table 3). Similarly, the mean pre-treatment ODI/NDI score were not significantly different when the two groups were compared based on LBP (p ¼ 0.93), NP (p ¼ 0.10), and NP and UBP (p ¼ 0.28) (Table 3). Based on pain location, the mean post-treatment NPRS (mean difference 1, p < 0.0001) and ODI/NDI (mean difference 6.2, p < 0.0001) scores, were significantly lower in the telerehabilitation group when compared to the control group in patients with LBP (Table 3). Similarly, the percentage of patients who achieved MCID of � 2 for NPRS (mean difference 7%, p ¼ 0.0004) and MCID of � 10 for ODI/NDI (mean difference 9.5%, p ¼ 0.002) scores were significantly higher in the telerahbilitation group when compared to the control group in patients with LBP (Table 3). However, there were no significant difference in the mean post-treatment NPRS (mean difference 0.3, p ¼ 0.34) and ODI/ NDI (mean difference 2, p ¼ 0.33) scores, and the percentage of patients who achieved MCID of � 2 for NPRS (mean difference 1.5%, p ¼ 1.00) and MCID of � 10 for ODI/NDI (mean difference 9.5%, p ¼ 0.20) scores when the two groups were compared in patients with NP (Table 3). Similarly, there were no significant difference in the mean post-treatment NPRS score (mean difference 0.9, p ¼ 0.05), and the percentage of patients who achieved MCID of � 2 for NPRS (mean difference 4%, p ¼ 1.00) and MCID of � 10 for ODI/NDI (mean difference 12.5%, p ¼ 0.41) scores when the two groups were compared in ups were compared in
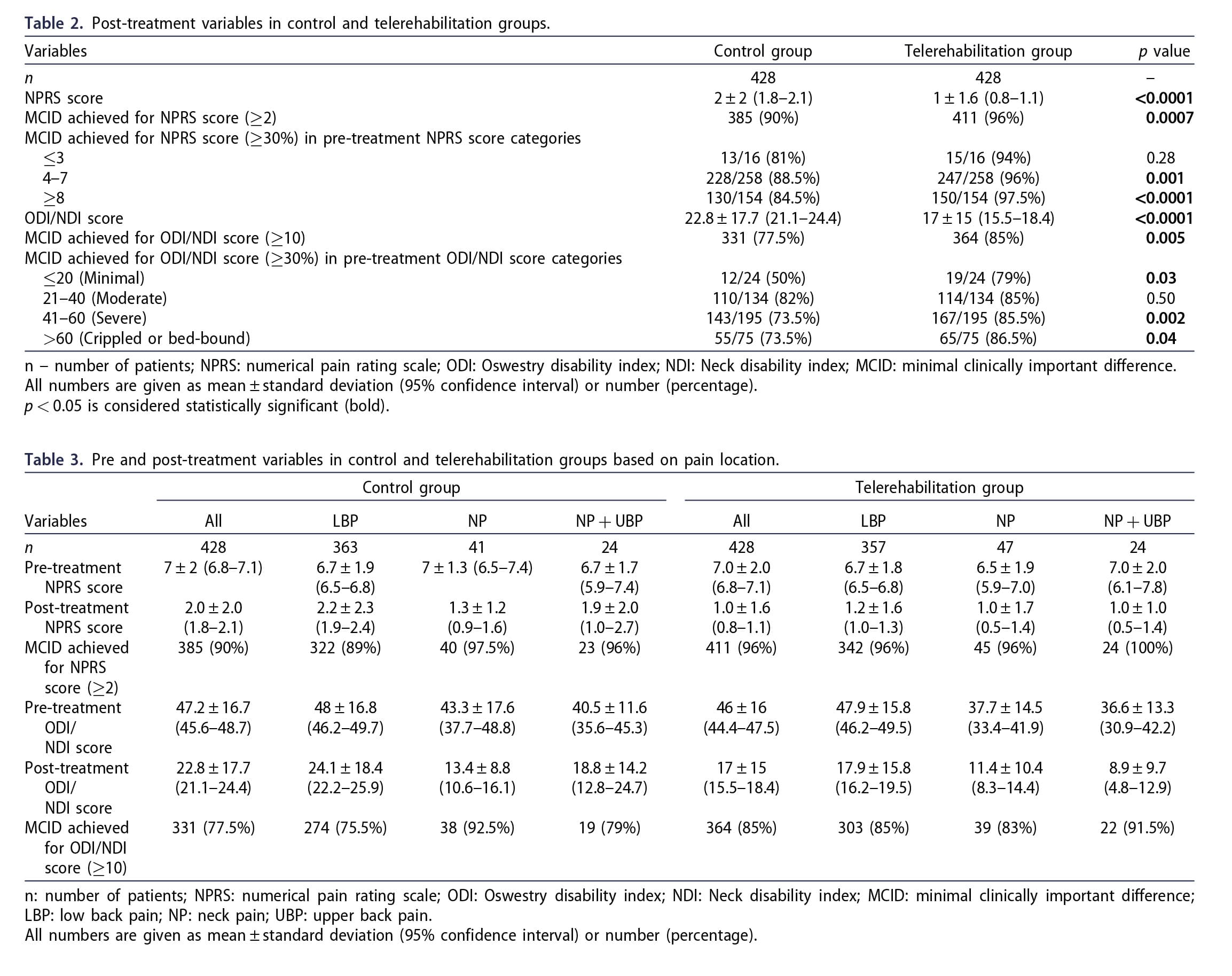
UBP (Table 3). The mean post-treatment ODI/NDI (mean difference 9.9, p ¼ 0.007) score was significantly lower in the telerehabilitation group when compared to the control group in patients with NP and UBP (Table 3).
The findings of our study indicate that telerehabilitation treatment showed significantly greater improvement in pain and disability when compared to in-clinic rehabilitation for spine pain. Although telerehabilitation has been reported to be effective in treating spine pain [4], few studies have compared its efficacy with inclinic rehabilitation treatment. Mbada et al. [11], in a comparative trial of teletreatment versus clinic-based MDT therapy in 47 patients with chronic LBP, reported no significant difference between the 2 groups in terms of pain and function at the end of 8 weeks. These findings were contrary to the findings of the current study where a significant difference was found in improvement in pain and disability between patients who underwent clinic-based multimodal rehabilitation treatment and patients who underwent telerehabilitation which used a combination of MDT therapy and core strengthening and stabilization exercises. A possible explanation for this difference in findings could be the greater number of subjects, patients with both lower back and neck pain, and patient with acute and chronic spine pain in the current study.
Home-based exercise programs for spine pain have their challenges which include poor compliance, absence of monitoring and feedback, and inability to incorporate the prescribed exercises in daily routine which can affect treatment outcome and increases the chances of recurrence [28,29]. Interestingly, in the current study, a significantly greater percentage of patients with severe pain (NPRS score �8) and with severe and crippling disability achieved MCID of 30% reduction in pain and disability in the telerehabilitation group when compared to the control group. This finding of significant improvement in clinical outcomes with telerehabilitation when compared to in-clinic rehabilitation has been confirmed by a recent double-blinded randomized control trial (RCT) by Ozden et al. [12], who reported more significant improvement in pain, function, quality-of-life, kinesiophobia, satisfaction, and motivation in the telerehabilitation group (n ¼ 25), which used a web-based telerehabilitation software, when compared with conventional rehabilitation group (n ¼ 25) at the end of 8 weeks of treatment for chronic LBP. Similarly, a recent study by Raiszadeh et al. [13], which compared clinical outcomes of clinic-based multidisciplinary therapy in an integrated practic unit (n ¼ 988) with online integrated multidisciplinary therapy (n ¼ 102) in individuals undergoing conservative care for LBP, reported greater pain relief and reductions in disability in the clinic-based therapy group and greater improvements in goal achievement in the online therapy group. However, Dadarkhah et al. [14], in an RCT comparing remote versus in-person exercise treatment for chronic non-specific LBP, reported no significant difference in pain and disability scores at the end of 3 months post intervention between the 2 groups which was contrary to the findings of the current study and could be explained by the smaller number of patients and the inclusion of only patients with chronic LBP in their study.
A possible explanation for a more significant improvement in pain and disability in the telerehabilitation group when compared to the in-clinic group could be that all patients in the telerehabilitation group were homebound or working from home due to the COVID-19 pandemic. Due to the lockdown, travelling to the clinic to receive treatment in the presence of significant pain and disability was avoided, their daily schedule was flexible, and the presence and support of family members during the treatment process, all of which may have improved compliance. Furthermore, the use of technology platforms to communicate about treatment steps and regular monitoring may have improved treatment adherence among the telerehabilitation patients by increasing the attractiveness of exercise programs, improving patient performance, and giving a sense of being supported by their caregiver due to improved communication and accessibility [30]
The application of telerehabilitation to treat patients with spine pain within the framework of ethical principles is essential for the protection of patient privacy. Ethical principles in telereahbilitation include universal accessibility, patient informed consent, respect of privacy, and professional confidentiality, and patient data safety [31,32]. The authors and all physical therapists who delivered telerehabilitation in the current study tried their best to ensure that the highest ethical standards were maintained. In the current study, all therapists involved in telerehabilitation were trained its ethical aspects which included taking informed consent, ensuring professional patient-care giver confidentiality during all communications, and patient data safety. Although no communication platform can be completely secure, patient-caregiver communication confidentiality and security was ensured using secure applications which were legally acceptable for delivering teletreatment during the COVID-19 pandemic lockdown [16]. Furthermore, none of the teleconsultation or treatment sessions were recorded to ensure patient confidentiality. Patient data safety was ensured by storing all patient related data in a proprietary electronic medical record (EMR) system developed and used only by our chain of clinics, and not in a commercially available EMR which allows third-party ownership and access to patient data. Furthermore, patient data access was given only to their care-givers involved in their telerehabilitation. To the best of our knowledge, this is the first and the largest propensity score-matched study in the literature, involving 856 patients with spine pain, which had compared the effectiveness of telerehabilitation during the COVID-19 pandemic with a previous cohort of in-clinic multimodal rehabilitation. However, this study had several limitations. First, the comparison of telerehabilitation data with retrospective data of in-clinic rehabilitation patients had its own biases and this study should be replicated as a prospective, randomized case-control study to confirm the effectiveness of telerehabilitation on spine pain. However, we have tried to reduce the effect of confounding factors such as age, gender, pre-treatment pain and disability, and treatment dose by using the propensity score matching method. Second, patients who were more comfortable using teleconference apps and had better internet connectivity would have been keener to seek telerehabilitation treatment which would have resulted in a selection bias. Third, a dedicated telerahbilitation software which has the facility to upload exercise videos would have been a more effective method to demonstrate various exercises [12], and was not used in the current study. However, various exercises were demonstrated by the treating therapist during each session and a digital document illustrating all the relevant exercises was shared with the patient for clarity and to be followed during home exercises. Finally, the restrictions in terms of work and travel imposed by the COVID-19 pandemic was a unique situation and may have been one reason for the excellent results achieved with telerehabilitation, better than in-clinic rehabilitation. Hence the findings of or study needs to be interpreted with caution and the efficacy of telerehabilitation needs to be confirmed with a high-quality study in future during non-pandemic times when all restrictions have been lifted and patients get back to their regular work and daily life routines.
Telerehabilitation achieved a significant reduction in pain and disability among patients with spine pain, better than in-clinic rehabilitation. These encouraging results during the COVID-19 pandemic indicate the need to further explore and test the efficacy and wider application of telerehabilitation for treating spine pain during non-pandemic times.
No potential conflict of interest was reported by the author(s).
The author(s) reported there is no funding associated with the work featured in this article.
Harshad Thakur http://orcid.org/0000-0003-3597-7113
Visit our nearest clinic for your first consultation