Request Appointment
Enter your details and we will be in touch with you shortly;
Or call
8655885566
between 8 am and 8 pm.

Sara Ansari, Gautam M. Shetty, Garima Anandani & C. S. Ram
Low back pain (LBP) is now the number one cause of disability globally with increasing annual health care and social costs due to lost wages and decreased productivity [1–3]. The role of interventional therapies and surgery is limited in the treatment of chronic LBP. The benefits of surgical procedures such as fusion surgery for non-radicular discogenic LBP may be modestly greater than non-surgical treatment options such as intensive rehabilitation [4–6]. Furthermore, surgery has a greater risk of adverse events and more expensive compared to non-surgical options [5]. Surgical procedures are primarily recommended for chronic lumbar radicular pain (LRP) [4–6], where pain is observed in the lower extremities along the course (dermatome) of a spinal nerve root with or without associated LBP and is caused by irritation or inflammation of sensory root or the dorsal root ganglion (DRG) of a lumbosacral spinal nerve [7,8].
Recent treatment guidelines for chronic LBP emphasise on physical and psychological therapies and self-management, and less emphasis on pharmacological and surgical treatment [6,9,10]. Several physiotherapeutic programmes have been used in conservative management of LBP including modalities such as electric stimulation, LASER therapy, and magnetic stimulation [11–16]. Kerr et al. [17] in an intent-to- treat analysis of a randomised observational cohort at 8 years showed no difference between surgical and non-operative treatment for the primary outcome measures such as SF-36 bodily pain, SF-36 physical function, and Oswestry Disability Index (ODI) in patients with intervertebral disc herniation and symptomatic radiculopathy. Although several studies have shown significant improvement in outcomes after physiotherapy in patients with LBP [17,18], the literature is lacking on the effectiveness of rehabilitation in patients who have been advised surgery for chronic LRP by their spine surgeons.
Hence, the purpose of our study was to determine the effectiveness of a structured physiotherapy protocol in patients with chronic LRP who were advised surgery by a spine surgeon based on their symptoms, clinical and magnetic resonance imaging (MRI) findings. We hypothesised that a structured physiotherapy protocol in patients with chronic LRP who were advised surgery by a spine surgeon will be effective in improving pain and disability and prevent surgery in such patients at a minimum follow-up of 12 months.
We retrospectively reviewed the records of 10043 patients treated for chronic LBP with a physiotherapy protocol at several centres of a clinic specialising in spine rehabilitation (QI Spine Clinic, India) from November 2016 to December 2018. For this study, the inclusion criteria were all patients who were advised surgery by a spine surgeon for chronic LRP with symptoms of at least 6 weeks or more at the time of presentation.
The advice of spine surgery was confirmed based on the spine surgeon’s prescription as provided by the patient during consultation at our rehabilitation clinic and the main underlying cause of chronic LRP was degenerative disc disease/disc herniation as reported on MRI and con- firmed by the spine surgeon’s prescription.
The exclusion criteria were patients with a follow-up of less than 12 months from the date of discharge and patients who have taken less than 30 days or more than 90 days of treatment. Based on the inclusion criteria, records of 530 patients who were recommended surgery by their spine surgeon were analysed out of which 237 patients who had a follow-up duration of less than 12 months and 104 patients who have taken less than 30 days or more than 90 days of treatment at our centres and were excluded. Hence, 189 patients were eligible for inclusion and were analysed in this study.
All patients were evaluated before and during the course of treatment. A thorough history of presenting complaints, past illness, previous surgical or non-surgical treatment or any red flag conditions (recent trauma or fall, night or at rest pain, fever, unexplained weight loss, progressive motor or sensory deficit, bowel or bladder symptoms, history of cancer, chronic steroid use, and immunosuppression) were recorded. Predominant findings of MRI reports in all patients were recorded.
The type of surgery prescribed by the patient’s spine surgeon was also recorded. All patients were clinically examined for posture, lumbar spine movement and flexibility, motor and sensory function (myotomal and dermatomal loss) by a physiotherapist in the clinic. Pain before and after treatment was recorded using the numerical pain rating scale (NPRS) and the severity of disability before and after treatment was recorded using the ODI [19,20].
The NPRS score was based on a numerical scale with pain intensity ranging from ‘0’ (no pain) to ‘10’ (worst pain imaginable) [19]. The ODI score was based on a patient-completed questionnaire containing ten topics including pain intensity and ability to perform various activities such as lifting, self-care, walking, sitting, standing, sleeping, travelling, sexual function, and social life and a total score ranging from ‘0’ (no disability) to ‘100’ (bed-bound) [20].
Pre- and post-treatment disability categories were deter- mined based on their ODI scores and were defined as minimal (0% to 20% ODI score), moderate (21% to 40% ODI score), severe (41% to 60% ODI score), crippled (61% to 80% ODI score), and bed-bound (81% to 100% ODI score) [20]. All patients were also evaluated diagnosed based on the Mechanical Diagnosis and Therapy (MDT) or McKenzie method as reducible or irreducible derangement, postural syndrome, dysfunction, or other (spondylolisthesis and stenosis) by a senior physiotherapist in the clinic [21].
A structured physiotherapy protocol based on MDT diagnosis was administered to each patient. Based on the severity of LBP on the NPRS scale during the first assessment, patients were advised bed rest or micro-current therapy for the first week if NPRS was ≤7. In such patients, once the pain on NPRS was 4–7 or in patients presenting with pain on NPRS 4–7, movement testing was done using the MDT method to determine directional preference. The patients were then advised directional movements that were performed under supervision by the treating physiotherapist and advised to be continued at home.
The patient was reviewed every week for progress or improvement in pain and function and once the pain on NPRS was <4, stabilisation exercises and device- based strengthening were performed [22]. A minimum of 6 supervised physiotherapy session at the clinic was advised to all patients to ensure patient compliance and accurate clinical review.
Treatment outcome of a patient was considered a full success if the patient shifts to a disability category of ‘minimal’ and pain NPRS of ≤1 and partial success if the patient improves in disability by one category (e.g.: shift from severe to moderate category) and pain NPRS of ≤3 after treatment. The treatment outcome of a patient was considered a failure if there was no change in the degree of pain or disability at the end of treatment.
As part of a follow-up review of this study, all patients were contacted by phone by one of the physiotherapists at the study centre. Patients were asked about any current symptoms, the current degree of disability based on ODI score, the severity of back pain using NPRS scale if present, any other treatment taken after discharge, any type of surgery done after discharge, and the satisfaction rate with results of treatment at our centre (as very satisfied, satisfied, neutral, dissatisfied, and very dissatisfied).
Pre- and post-treatment demographic and clinical outcome data of 189 patients were analysed for this study. Pre and post-treatment clinical outcome parameters such as NPRS, ODI, and change in the disability category were compared to determine the effectiveness of treatment. Categorical data were compared using Fisher’s test and continuous data were compared using the t Test. A p value of <0.005 was considered significant. Statistical analysis was performed using the PRISM software, version 6 (GraphPad Software, San Diego, CA).
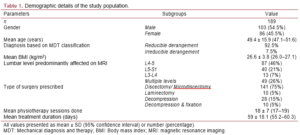
Demographic data of the study population is summarised in Table 1. One hundred and seventy-five patients (92.5%) who were prescribed surgery were diagnosed as reducible derangement and 14 patients (7.5%) were diagnosed as mechanically unresponsive radiculopathy based on the MDT method. On MRI, a majority of the patients (78%) had an intervertebral disc bulge, protrusion, herniation or extrusion with the L4-5 vertebral level most commonly affected (46%) (Table 1). Discectomy or microdiscectomy was the most common surgical procedure prescribed (75%) to the patients by their spine surgeon (Table 1).
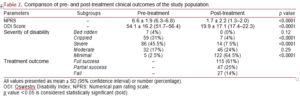
After a mean 18 (range, 6–49) sessions and mean 59 days (range, 30–90 days) duration of treatment, there was a significant reduction (p < 0.0001) in the mean NPRS score (Table 2). Similarly, there was a significant reduction (p < 0.0001) in the ODI score after treatment (Table 2). There was a significant reduction in the percentage of patients in the crippled (p < 0.0001) and severe (p < 0.0001) disability categories and a significant increase in the percentage of patients in the minimal disability category (p < 0.0001) after treatment (Table 2). At the time of discharge, 86% of patients were considered a full or partial success for the treatment out- comes (Table 2).
Of the 189 patients contacted, 89 patients (47%) responded and could answer queries about their current clinical and functional status. At a mean follow-up of 18 ± 4.1 months (range, 12–28 months), 9 patients (10%) had undergone lumbar surgery. The mean NPRS score, as reported by the patient during the follow-up call, was 2.1 ± 2.4 (0–9) and 56 patients (63%) had minimal disability as per the ODI score and 52 patients (58.5%) reported no pain or complaints related to their lower back. Sixty-six patients (74%) were either very satisfied or satisfied with the outcome of their treatment.
The purpose of this study was to determine the effectiveness of a structured physiotherapy protocol in patients with chronic LRP who were advised surgery by a spine surgeon based on their symptoms, clinical and MRI findings. The main finding of our study was that patients who were prescribed lumbar surgery by their spine surgeon for chronic LRP had significant improvements in their pain and disability in terms of NPRS and ODI scores at the end of two months of physiotherapy treatment. Furthermore, these improvements could still be seen in the majority of patents at a minimum follow-up of one year with 74% of patients reporting to be satisfied or very satisfied with their treatment, and only 10% (9/89 patients) of patients undergoing lumbar spine surgery at a mean follow-up of 18 months.
These findings were similar to a prospective cohort study conducted by Svensson et al. [23] on 41 patients who qualified for lumbar disc surgery for chronic LBP and were treated conservatively by a structured physiotherapy treatment model where 11% patients (4/36 patients) had undergone surgery at the end of 2 years. Similarly, Nelson et al. [24] in a study of 62 patients who were recommended surgery by their physicians for their low back or neck pain and underwent exercise rehabilitation and specific isometric strength testing using equipment, reported a surgery rate of 8% (3/38 patients) at a mean follow-up of 16 months.
However, results of randomised trials comparing surgical vs non-operative treatment for lumbar disc herniation published in the literature reported a higher rate of conversion to surgery in patients treated non-operatively for chronic LBP [25,26]. The reason for higher conversion rates to surgery in these studies was probably due to the type of physiotherapy used in treating patients. The non-operative treatment groups in these studies received a variety of different treatment methods unlike the current study where a structured physiotherapy protocol was used for patients.
There is no evidence on a particular type of exercise therapy being more effective than others in the treatment of chronic non-specific LBP [27]. Lam et al. [28] in a literature review and meta-analysis reported that moderate- to high- quality evidence in the literature suggesting that MDT is superior to other rehabilitation interventions for reducing pain and disability in patients with chronic LBP. Our rehabilitation protocol was designed in a structured manner and involved a greater emphasis on pain control using directional movements and trunk stabilisation and device-based strengthening exercises.
Furthermore, patients were advised ergonomic/strengthening exercises to be continued at home after discharge to prevent the recurrence of symptoms. This could be a reason why 58.5% of patients were symptom- free at a mean follow-up of 18 months. The prospective study by Svensson et al. [23] confirms that a structured physiotherapy treatment protocol can help reduce symptoms and prevent surgery during the first 2 years after discharge. However, they used MDT principles with graded trunk stabilisation training to achieve these outcomes whereas patients in the current study were also treated with device-based strengthening exercises that have been reported to be effective in the treatment of LBP [22,23].
There are several limitations to this study. First, a retrospective analysis has the disadvantage of inherent limitations and biases. Second, it is difficult to determine whether good clinical outcomes, at a mean follow-up of 18 months, seen in our patients were the result of our structured physiotherapy protocol or due to the natural healing process. A majority of patients in the current study showed significant improvement in clinical outcomes at the end of 2 months of treatment.
Since these outcomes were still present at a minimum follow-up of 12 months, it is unlikely that the natural healing process was responsible for the positive outcomes in our patients. Finally, a well-designed, prospective randomised trial needs to be undertaken to further confirm the benefits of a structured physiotherapy protocol for the treatment of chronic LRP which might be effective in preventing surgery.
Although a surgical procedure like lumbar discectomy has been reported to be more effective than conservative management in alleviating symptoms due to lumbar disc herniation refractory to initial conservative management [29], several factors such as the type of surgery conducted [30], MRI findings [31], duration of symptoms and time since surgery [17] may affect the outcome of surgical intervention. Recent clinical practice guidelines suggest that most surgical procedures used for treating lumbar spine conditions lead to similar outcomes as non-invasive treatment modalities [4,32].
Furthermore, surgical and interventional procedures should be reserved for patients with persistent and disabling spinal pain that fail to improve with non-invasive treatment. The decision to treat chronic LRP with elective surgical procedures should be based on the estimated benefits when com- pared to the cost involved and the risk of complications, especially in low-income countries where resources are limited [32,33].
In conclusion, a multi-modal physical rehabilitation protocol is effective in significantly improving pain and disability in patients indicated for surgery for chronic LRP. At a minimum follow-up of 12 months, pain and disability continued to be significantly lower, the majority of the patients continued to be symptom-free and 10% of patients underwent lumbar surgery. A structured, multi-modal physiotherapy protocol is effective for the treatment of chronic LRP in patients indicated for surgery and may help prevent surgery in the short-term.
Visit our nearest clinic for your first consultation